Key facts you should know about the Burundi Health System
Briefing Issue #66, Friday, April3, 2020

Dear Readers,
Today the most robust health systems in the world are challenged by unprecedented crises due to Coronavirus. Burundi’s vulnerability to COVID-19 where the onset of other diseases is high and the Burundian Government has taken certain actions to mitigate the risks.
To date, the Burundian government's efforts to stop or slow down COVID-19 in the country have been largely limited to the control of travelers coming out of the country.
Measures implemented to avoid or limit the spread of COVID-19 decreed on March 24, 2020, include:
quarantine since March 6, 2020, of all passengers from affected countries;
the suspension, of all international flights from March 21, 2020, except flights related to the transport of goods, medical evacuations, humanitarian and diplomatic actions;
the suspension of all official international missions;
the suspension from March 19, 2020, of the granting visas to enter Burundi, and the encouragement of citizens to practice social distancing.
To date, Burundi has not yet decreed measures to close schools or places of worship and to ban sporting events or limit public gatherings, etc., similar to those which have been decreed in many affected countries all over the world.
To fulfill our mission of filtering the news, bringing to you concise information about game-changing events and insights that may help you make better decisions in your professional and personal life, this Friday we present to you key facts you should know about the Burundi Health System.
1.Health system structure
Burundi's health system is organized into three levels:
Level (1): the central level ensures the development of policies and strategies, planning, resource mobilization, management, monitoring and evaluation of performance, regulation, and coordination of the sector.
Level (2): the intermediate level with 17 provincial offices responsible for coordination and support to districts. It ensures equitable distribution and efficient use of resources to districts. As part of his responsibilities, the Medical Director of the health province advises the Provincial Governor on health matters.
Level (3): The peripheral level is represented by the health district considered as the basic operational entity of the national health system. It consists of an administrative base, a district hospital, and a network of public, licensed, or private health centers.
2.Health indicators
Burundi has a population density of 437 people per square kilometer and is experiencing continuously high population growth.
In 2018, the average birth rate was 5.5 children per woman – one of the highest birth rates in the world.
Burundi’s health indicators lag behind those of the rest of Sub-Saharan Africa . Life expectancy at birth (56 years) is ranked among the lowest in the world and is two years below the average of Sub-Saharan Africa.
The under-five mortality rate decreased from 152 per 1,000 live births in 2000 to 81.7 per 1,000 live births in 2015. With such a ratio, Burundi is ranked among the highest decile of the global distribution, along with countries such as the Central African Republic and the Democratic Republic of Congo.
Maternal mortality remains very high in Burundi despite the reduction from 954 per 100,000 births in 2000 to 712 per 100,000 births in 2015 (World Development Indicators 2015).
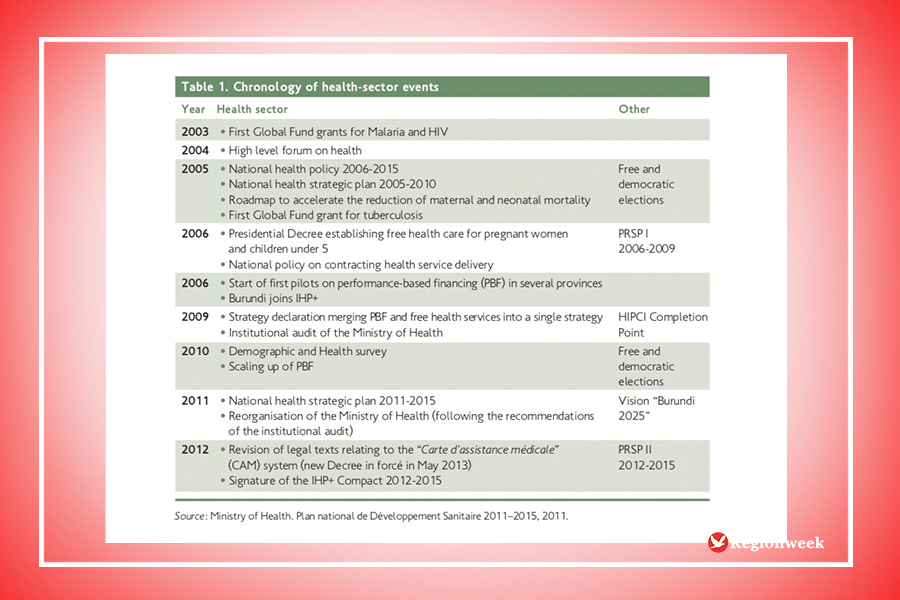
3.The health policy framework
The health policy framework of the health sector in Burundi has gradually been strengthened, and the country is quite advanced compared to many others (in Sub-Saharan Africa And elsewhere) in terms of introducing new and far-reaching policy reforms.
One important example of this was the introduction of a national policy of Free Health Care for pregnant women and under-5 children as well as a national policy of contracting in 2006.
Other important strategies and policies have also been introduced for other key areas within the health sector, e.g. for human resources, decentralization and the creation of health districts.
Burundi has adhered to the various world and regional frameworks for collaboration, in particular IHP+, Harmonization for Health in Africa, the Busan High-Level Forum on Aid Effectiveness, and the Commission on Information and Accountability for Women’s and Children’s Health.
If you wish to support this Newsletter we created a $5/Month subscription plan, you can join our Premium community of supporters by clicking here
4.Health sector budget

Compared to other low-income countries in Africa, the Government of Burundi dedicates a large share of its budget to the health sector mainly because of its commitment to Free Health Care.
The share of the Government budget allocated to health increased from 5.3 percent in 2007 to 10.41 percent in 2010. However, since 2010, this indicator has not increased significantly and has not yet reached the Abuja declaration target (15 percent).
Between 2010 and 2013, there was an increase in current expenditure on health, which rose from BIF 286 billion in 2010 to BIF 390 billion in 2013.
Nevertheless, total health expenditure (THE) per capita in real terms first increased between 2007 and 2010 from BIF 18,848 to BIF 23,777 and then decreased to BIF 20,631 in 2013 (US$29.93).
Per capita expenditure is far from US$56 of THE per capita per year recommended by the Taskforce on Innovative Financing for Health Systems to ensure the provision of basic health services.
According to the National health policy 2016-2025 of Burundi, National Health Accounts (2010), the contribution of households covers about 30% of health expenditure.

According to Financial Law 2017, 48.6 percent of allocations to the Ministry of Public Health comes from a few donors. Belgium provides its support to a wide range of activities, and the USA concentrates on vaccination, UNICEF on infantile health and the European Union on construction efforts.
In 2017, external support represents nearly half of allocations to the Ministry of Health, but still below the level of support of 60.1 percent in 2015. High recurrent costs limit investments: only around 7% of national resources are investments, and the grand majority of resources are recurrent costs, such as salaries. Investments are nearly entirely financed through external resources.
5.Human resources for health
Burundi has inadequate human resources for health with an impact on the quality of care. The country has an average of 1 medical doctor per 20,865 inhabitants and 1 nurse per 1,542 inhabitants (compared to 1 per 3,703 and 1 per 806, respectively, in Africa). Moreover, there is an inequitable distribution of health workers with fewer of them working in rural areas (50.5 percent of physicians and 21 percent of nurses are in Bujumbura).
The number of doctors went from 200 (in 2007) to 554 (in 2013) 51 bringing the ratio to 1 doctor per 16,368 inhabitants (WHO recommends 1 Doctor per 10,000 inhabitants).
In 2013, Burundi had 6,573 nurses all categories combined carrying the ratio 1 nurse per 1,380 inhabitants (WHO recommends 1 per 3,000 inhabitants) although 61% (4,005) of this workforce is made up of insufficiently qualified auxiliaries.
As in several other African countries, the problem of brain drain arises for medical specialists (around 150 Burundian medical specialists continue to work outside the country).
6.Infrastructures

Between 2005 and 2013, the number of Health Centers known as Centre de Santé (CDS) rose from 573 in 2005 to 89,749 in 2014, i.e. 324 CDS built in 10 years with an average of 32.4 CDS built / year.
During the same period, the number of hospitals increased from 44 in 2005 to 69 in 2014, ie 25 more hospitals in 10 years with an average of 2.5 hospitals built / year; which brings the ratio respectively to 1 CD for 10,109 inhabitants (WHO: 1 CDS / 10,000 inhabitants) and 1 Hospital for 131,414 inhabitants (WHO: 1 hospital for 150,000 inhabitants).
Currently, Burundi has two national reference laboratories that comply with standards [INSP and CHU Kamenge Laboratories] and members of the East African Community (EAC) laboratory network.
Burundi has 4 functional regional blood transfusion centers (Cibitoke, Gitega, Bururi, and Ngozi).
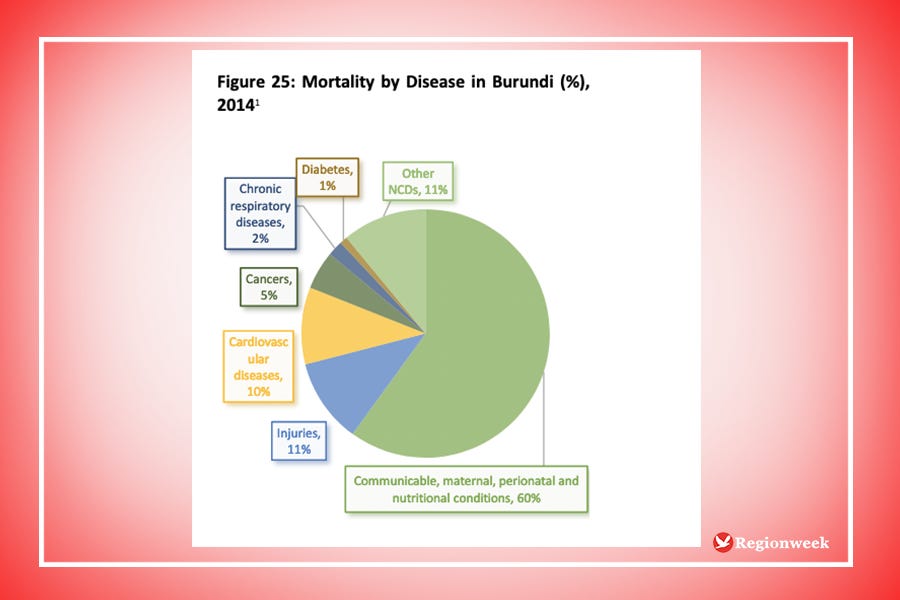
7.Diseases with epidemic potential
In Burundi, diseases with epidemic potential under surveillance are measles, cholera, meningococcal meningitis, malaria, acute flaccid paralysis (PFA), viral hemorrhagic fevers (Ebola, Lassa, and Marbourg), measles and neonatal tetanus.
In recent years, Burundi has faced a series of cholera epidemics. The last measles epidemic dates back to 2011 as the country strengthened routine immunization with a mass measles campaign in 2012 and the introduction of the second dose of measles vaccine in 2013.
8.Hygiene and environmental sanitation
Hygiene and environmental sanitation are still precarious and expose populations to the contamination of infectious diseases of different natures. The water problem does not exist in terms of quantity in Burundi. However, even if there are many sources of water, access to quality water, essential for good health, is not guaranteed for a relatively large part of the population.
Access to drinking water services remains low due to an uneven distribution of water resources and population growth which accentuates the pressure on this resource. Having taken the measure of the issues at stake, the Governments is resolutely engaged in a process leading to the adoption and promulgation of the “National Water Policy” following a reflection involving all the actors in the water field.
9.The national health insurance scheme
Burundi is a low-income country, it has not achieved universal health coverage (UHC) yet. Access to adequate and affordable health care is difficult for 90% of the Burundian population of the informal sector who live mainly in rural areas.
The Medical Assistance Card (CAM) and Mutuelle de la Fonction Publique (MFP) are functional since 1980. The Ministry of Health subsidizes first-line antimalarial drugs, ARVs, anti-tuberculosis drugs, and certain drugs against Neglected tropical diseases. Community mutuals target around 2% of the population.
Informal workers aged 21 or older can buy a Medical Assistance Card for 3,000BIF a year and pay 20% of the cost of medicine and 20% of the cost of medical appointments and tests in local clinics and district hospitals.
The public-sector mutual provides medical benefits for civil servants and covers 80% of medical costs, 70% for medicine, and 90% for chronic diseases. Civil servants contribute 6% of salaries (excluding housing expenses). A private-sector mutual was established in May 2014 but is not functional yet.
The Bottom Line
While Burundi has made good strides in building hospitals, in the COVID-19 context it barely has intensive care units that would care for the very sick that may require admissions. Yes, the virus threatens the economy on a serious tone but the strength of the economy is based on a healthy working force. Even countries with powerful health systems are hit with the virus, there is a need to quarantine people as much as possible, radical measures are crucial now, or Burundi may be overwhelmed and might lose the battle.
“We know how to bring the economy back to life. What we do not know is how to bring people back to life”- President Akufo-Addo
A struggling economy can always be revived but dead lives never come back
Stay safe!
Fabrice Iranzi
Editor, RegionWeek.com
If you wish to support this Newsletter we created a $5/Month subscription plan, you can join our Premium community of supporters by clicking here
Resources for further readings and notes
http://minisante.bi/wp-content/uploads/politiques/Politique%20Nationale%20Sante%202016%202025%20VF%2021052016.pdf
https://www.unicef.org/esaro/UNICEF_Burundi_--_2017_--_Health_Budget_Brief.pdf
https://apps.who.int/iris/bitstream/handle/10665/137042/ccsbrief_bdi_en.pdf;jsessionid=8B495791F0DF4851687CB862305A798F?sequence=1
https://www.usaid.gov/burundi/global-health
http://minisante.bi/wp-content/uploads/politiques/covid19/Projet%20de%20pr%C3%A9paration%20et%20de%20riposte%20strat%C3%A9gique%20du%20Burundi%20face%20au%20COVID-19_Plan%20de%20Mobilisation%20de%20Parties%20Prenantes%20(PMPP).pdf
http://minisante.bi/wp-content/uploads/politiques/covid19/Projet%20de%20pr%C3%A9paration%20et%20de%20riposte%20strat%C3%A9gique%20du%20Burundi%20face%20au%20COVID-19_Plan%20d'engagement%20environnemental%20et%20social%20(pees).pdf
https://www.hhrjournal.org/2018/05/a-comparison-of-health-achievements-in-rwanda-and-burundi/
https://internationalmedicalcorps.org/country/burundi/
https://cdn1.internationalmedicalcorps.org/wp-content/uploads/2020/01/CS2020_Burundi_v01.14.2020.pdf
http://documents.worldbank.org/curated/en/838321488164451748/pdf/Burundi-Health-PAD-02062017.pdf
RegionWeek is a Burundi-based media for a new generation of achievers in Africa, a platform devoted to chronicling the journey to Freedom and Empowerment.



